Stephanie KY Choi, Ester Lazzari, Christos Venetis and Georgina Chambers

With rising infertility and increasing demand for fertility treatments globally, understanding the role of medically assisted reproduction (MAR) in population demographics and family formation patterns has never been more important. Stephanie KY Choi, Ester Lazzari, Christos Venetis and Georgina M. Chambers document the role played by all common forms of MAR treatments on completed family size and birth timing in Australia.
Over the past generation, fertility treatment has been revolutionized by the advent and development of assisted reproductive technologies (ART), such as in vitro fertilization (IVF). These technologies have accounted for 4-5% of the Australian total fertility rate each year over the last decade (Lazzari et al. 2021). Unlike other forms of fertility treatments like ovulation induction (OI) and intrauterine insemination (IUI), ART involves fertilization outside the body (in vitro), followed by the transfer of resulting embryos into the uterus, with the aim of achieving a pregnancy. Together, ART, OI, and IUI are often referred to as medically assisted reproduction (MAR).
Although national ART registries provide some insights into the contribution of ART to the number of births in a country, little is known about their role, along with other forms of MAR, on childbearing timing and family size. This represents a significant gap in demographic and population policy knowledge, particularly given the growing evidence of rising infertility due to childbearing postponement (Habbema et al. 2015). At the same time, the use of fertility treatments is increasing globally (Chamber et al. 2021b), and several countries are showing a growing interest in subsidizing ART treatment as a pronatalist policy to counteract fertility decline (Gray et al. 2022).
In a recent study (Choi et al. 2023), we investigated how the mode of the conception of the firstborn child, whether through MAR or natural conception and the mother’s socioeconomic status impact on family formation, including childbirth timing (postponement and recovery) and completed family size.
We used a unique longitudinal Australian dataset covering all major forms of MAR to examine their contribution to these fertility dynamics (Chambers et al. 2021a). Australia provides an ideal setting to explore the potential impact of MAR on family formation, as funding for MAR treatment is supportive, and utilization rates are relatively high (Chambers et al. 2021b).
Completed family size and mean age at first birth by mode of conception
Mothers who used MAR treatment to conceive their firstborn child were older and had a smaller completed family size by the end of their reproductive lives than mothers giving birth to their first child naturally. This effect was more pronounced among mothers who used ART compared with those who used more traditional fertility treatments, such as OI and IUI. In particular, the mean maternal age at first birth was higher for ART mothers: 34.6 years vs 31.0 years for OI/IUI mothers and 28.7 years for mothers of a naturally conceived child. Moreover, ART mothers achieved a smaller completed family size: 2.20 children against 2.98 and 3.23, respectively, for OI/IUI mothers and mothers of naturally conceived children.
Fertility postponement and recuperation by mode of conception
Figure 1 illustrates the patterns of fertility postponement and recovery for mothers who had fertility treatment and those who conceived naturally. The comparison with the reference group of natural-conception mothers enables the visualization of the gap in completed family size between different groups of mothers by mode of the conception of their firstborn child over their reproductive ages.

Mothers who had fertility treatment (ART and OI/IUI) had 0.68 and 0.24 fewer children, respectively, than natural-conception mothers. Additionally, ART mothers postponed childbearing for longer than those who underwent OI/IUI. ART mothers had their first child at age 36.4 years, versus 30.3 years for OI/IUI mothers.
The impact of maternal socioeconomic status
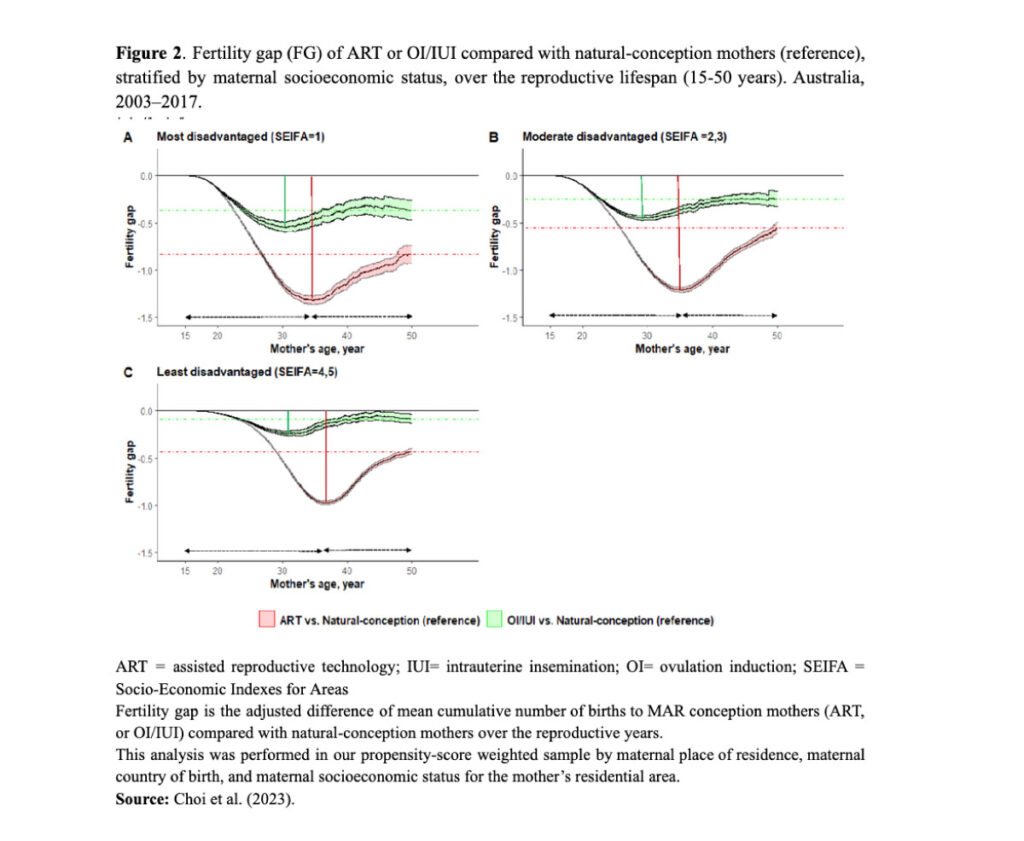
Mothers residing in more socioeconomically advantaged areas who used ART to conceive their firstborn child were about 3 years older than ART mothers residing in less advantaged areas. Despite this age difference, the fertility gap with respect to mothers conceiving their first child naturally was smaller for ART mothers in more advantaged areas than for ART mothers in less advantaged areas (0.43 fewer children versus almost one less child, respectively) (Figure 2). For OI/IUI mothers on the other hand, by the end of the reproductive years, the impact of maternal socioeconomic status on the fertility gap with respect to mothers conceiving their first child naturally was relatively small (Figure 2).
Missed births and reproductive inequalities
The enduring discrepancy in the final number of children among mothers who used ART or other types of fertility treatments for their first birth and those who conceived naturally highlights the importance of understanding the natural decline in fertility with age, as well as the limitations of relying on MAR in achieving a desired family size. There is a pressing need to enhance awareness and education on these issues.
It is also worth noting that not only the mode of conception but also the mother’s level of socioeconomic advantage influences family formation dynamics. The smaller completed family size of mothers of lower socioeconomic status compared with mothers of higher socioeconomic status – despite both conceiving their firstborn child through ART and the latter starting their families on average three years later – suggests the existence of continued socioeconomic inequalities in the ability to achieve the desired family size through ART, even in countries with supportive funding environments like Australia.
References
- Chambers, Georgina M, Choi, Stephanie KY, Irvine, Katie, Venetis, Christos, Harris, Katie, Havard, Alys, Norman, Robert J, Lui, Kei, Ledger, William, and Jorm, Louisa R. (2021a). A bespoke data linkage of an IVF clinical quality registry to population health datasets; methods and performance. International Journal of Population Data Science, 6(1): 1679.
- Chambers, Georgina M, Dyer, Silke, Zegers-Hochschild, Fernando, de Mouzon, Jacques, Ishihara, Osamu, Banker, Manish, Mansour, Ragaa, Kupka, Markus S, and Adamson, David G. (2021b). International Committee for monitoring assisted reproductive technologies world report: assisted reproductive technology, 2014. Human Reproduction, 36(11): 2921-2934.
- Choi, Stephanie KY, Lazzari, Ester, Venetis, Christos, and Chambers, Georgina M. (2023). Childbirth timing and completed family size by mode of conception – the role of medically assisted reproduction: a population-based cohort study in Australia. The Lancet Regional Health Western Pacific
- Gray, Edith, Reimondos, Anna, Lazzari, Ester, Breunig, Robert, Steinhauser, Ralf, Zhang, Jacquelyn, Biddle, Nicholas, and Gray, Matthew. (2022). Impact of policies on fertility rate.
- Habbema, J Dik F, Eijkemans, Marinus J C, Leridon, Henri, and te Velde, Egbert R. (2015). Realizing a desired family size: when should couples start? Human Reproduction, 30(9): 2215–2221.
- Lazzari, Ester, Gray, Edith, and Chambers, Georgina M. (2021). The contribution of assisted reproductive technology to fertility rates and parity transition. Demographic Research, 45(35): 1081–1096.
No comments:
Post a Comment