International migration from Africa to France and contraception use

An original multi-sited analysis of migration (from selected sub-Saharan African countries to France) and contraceptive use reveals that migrant women align more closely with native French women than women in origin countries, a finding that has important implications for prevention of undesired pregnancies. Julia Behrman interprets this as a sign of the potential adaptation of migrants to the new contraceptive environment.
Is there evidence of contraceptive adaptation among African migrants to France, away from the practices they used in their origin countries? There are many reasons why this type of adaptation may take place. For example, migrants encounter changes in reproductive healthcare access and the prevalence and availability of contraceptive methods, different norms about method acceptability, new employment opportunities, and reunification with other family members (including spouses).
Research on the relationship between international migration and modern contraceptive usage often compares immigrants to natives, ignoring what happens in origin countries (Ochako et al. 2016; Akinyemi, Odimegwu, and Adebowale 2017; Tapales, Douglas-Hall, and Whitehead 2018). Unfortunately, this one-sided approach cannot tell us much about the relative distance of migrants from these two potential terms of comparison and therefore, indirectly, about their adaptation to the new contraceptive environment. To overcome this limitation and understand whether migration is associated with changes in contraceptive usage, in a recent paper we adopted a multi-sited approach that includes data on individuals in both sending and receiving countries (Behrman et al. forthcoming). Reproductive health outcomes are rarely explored using a multi-sited approach. Existing scholarship that combines data sources focuses on country-level comparisons of fertility differences (Toulemon 2004; Dubuc 2012). Only a handful of studies combine individual-level data from origin and destination contexts to examine fertility (Singley and Landale 1998; Lübke 2014; Impicciatore, Gabrielli, and Paterno 2020) and none of these explores contraceptive outcomes.
We standardized and integrated data from two different sources, one collected in France (destination) and the other collected in six West and Central African countries (origin) between 2006 and 2012. The six sending countries (Cameroon, Côte d’Ivoire, Mali, Senegal, Congo Brazzaville, and Congo DRC) all had – and still have – higher fertility and lower usage of modern contraception than France in 2008-2009, thus making this an interesting setting for comparison.
Data and methods
The data in the analysis come from two sources: the Trajectories and Origins Survey (TeO) and the Demographic and Health Surveys (DHS). TeO was conducted by the French Institute for Demographic Studies (INED) and the French National Institute of Statistics and Economic Studies (INSEE) between September 2008 and February 2009. The DHS is conducted throughout sub-Saharan Africa by host country governments in collaboration with ICF International. We use DHS data collected between 2006 and 2012 (Table 1)1.

This combined dataset includes information on three groups of women:
A) Non-migrant French women;B) Women who migrated to France after age 15 from the six West and Central African countries mentioned above;C) African women in those same countries.
The challenge for this type of analysis is that migrants are selected: this means that African women in France may be (profoundly) different from those who remain in the origin country. They do, in fact, have higher average levels of education and come from smaller families than their non-migrant counterparts. As they differ in several respects, these migrants could have used different types of contraception from their compatriots even if they had stayed home. We addressed this potential source of bias with a weighting methodology that enabled us to compare “like with like” in terms of education, age, religion and other observable background characteristics.
Adaptation in contraception
Figure 1 presents the predicted probabilities of different types of current contraceptive usage among the three groups of interest listed above.
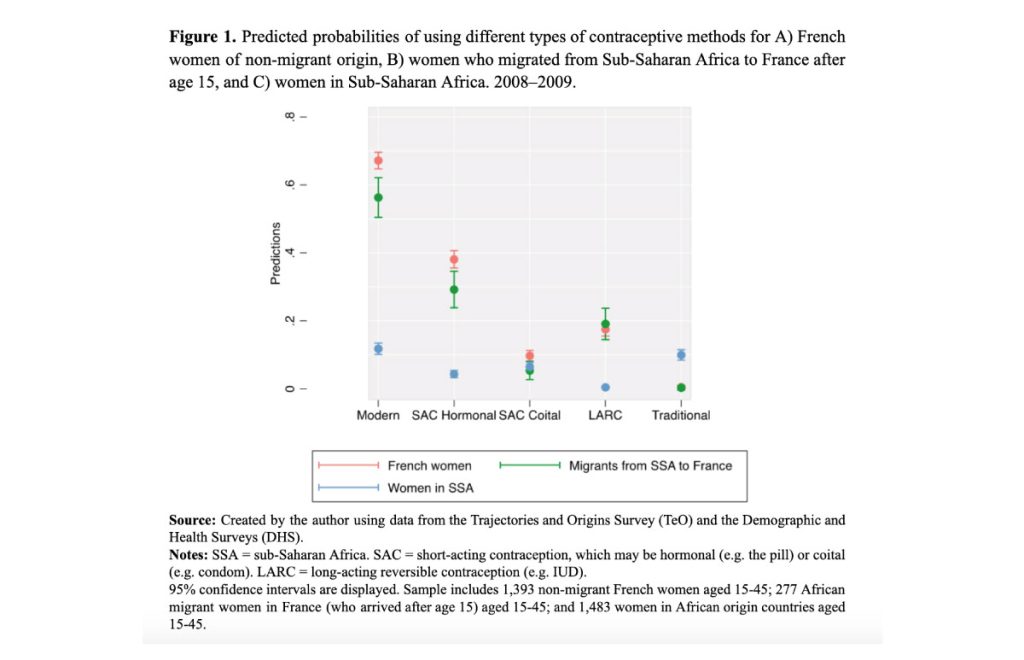
Our findings indicate that the contraceptive practices of female African migrants in France resemble more closely those of French women than those of women in African origin countries. For example, a predicted 56% of African migrants to France use a modern method of contraception compared to 67% of French women and 11% of women in the corresponding countries of origin. Similar patterns hold for current use of hormonal short-acting contraceptive (38% of French women, 29% of African migrant women in France, 4% of women in the six African origin countries) and long-acting reversible contraception (18% of French women, 19% of African migrant women, less than 1% of women in the six African origin countries). Finally, use of traditional contraceptive methods is significantly higher among women in the African countries of origin (10%) than in the other two groups (0%).
More refined (multivariate) analyses confirm these findings, and suggest that migration is associated with the following changes in probability of current usage of contraception (in comparison to women in origin countries):
+36 percentage points for modern methods,+20 percentage points for hormonal short-acting contraception,+17 percentage points for LARCs, and‒10 percentage points for traditional methods.
Conclusions
Unfortunately, our analysis suffers from a few limitations. First due to the difficulties of locating data with adequate samples of migrants and appropriate information on reproductive health, we must rely on an older data source. Nonetheless, there are no reasons to believe that the contraceptive adaptation process of migrant women outlined above has changed in any significant way in the past 10‒15 years. Second, we could not control for unobserved characteristics such as gender ideology, religiosity, and contraceptive attitudes, which may influence both likelihood of migration and contraceptive usage.
This notwithstanding, our findings support the general idea that migrant women adapt to the new context (in terms of rules, practices, habits, etc.), and, in this specific case, tend to adopt the contraceptive norms that are prevalent in the destination country.
Migrant women’s contraceptive access and usage should feature more prominently in discussions of migrant fertility. Among policymakers, there is a need for more attention to reproductive policies that make effective forms of contraception widely available to migrant populations in a way that is culturally sensitive and attentive to their reproductive needs.
Acknowledgments
This work is supported with grant SES 1918274 from the National Science Foundation to Drs. Julia Behrman and Abigail Weitzman and is also supported by grant, P2CHD042849, Population Research Center, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
We are grateful to the Centre Maurice Halbwachs for granting access to the data [Trajectoires et origines (TEO)— version complete—2008: (2008, fichier electronique), INED et INSEE (producteur), Centre Maurice Halbwachs (CMH, diffuseur)]
Footnotes
1The DHS can be accessed at: https://dhsprogram.com/ and TeO can be accessed at: http://quetelet.progedo.fr/.References
- Akinyemi, Joshua O., Clifford O. Odimegwu, and Ayo S. Adebowale. 2017. “The Effect of Internal Migration, Individual and Contextual Characteristics on Contraceptive Use among Nigerian Women.” Health Care for Women International 38 (10): 1075–94. https://doi.org/10.1080/07399332.2017.1345908.
- Behrman, Julia A., Michelle A. Eilers, Isabel H. McLoughlin Brooks, and Abigail Weitzman. Forthcoming. “International Migration and Modern Contraceptive Use: A Research Note on African Migrants to France.” Demography. https://doi.org/10.1215/00703370-9611478.
- Dubuc, Sylvie. 2012. “Immigration to the UK from High‐Fertility Countries: Intergenerational Adaptation and Fertility Convergence.” Population and Development Review 38 (June): 353–68.
- Impicciatore, Roberto, Giuseppe Gabrielli, and Anna Paterno. 2020. “Migrants’ Fertility in Italy: A Comparison Between Origin and Destination.” European Journal of Population 36 (4): 799–825. https://doi.org/10.1007/s10680-019-09553-w.
- Lübke, Christiane. 2014. “How Migration Affects the Timing of Childbearing: The Transition to a First Birth Among Polish Women in Britain.” European Journal of Population / Revue Européenne de Démographie 31 (1): 1–20. https://doi.org/10.1007/s10680-014-9326-9.
- Ochako, Rhoune, Ian Askew, Jerry Okal, John Oucho, and Marleen Temmerman. 2016. “Modern Contraceptive Use among Migrant and Non-Migrant Women in Kenya.” Reproductive Health 13 (1): 67. https://doi.org/10.1186/s12978-016-0183-3.
- Singley, Susan G., and Nancy S. Landale. 1998. “Incorporating Origin and Process in Migration-Fertility Frameworks: The Case of Puerto Rican Women.” Social Forces 76 (4): 1437–64. https://doi.org/10.1093/sf/76.4.1437.
- Tapales, Athena, Ayana Douglas-Hall, and Hannah Whitehead. 2018. “The Sexual and Reproductive Health of Foreign-Born Women in the United States.” Contraception 98 (1): 47–51. https://doi.org/10.1016/j.contraception.2018.02.003.
- Toulemon, L. 2004. “Fertility among Immigrant Women: New Data a New Approach.” Population and Societies, no. 400 (January): 1–4.
source figure 1: The world bank
No comments:
Post a Comment