Researchers are struggling to tally mortality statistics as the pandemic rages. Here’s how they gauge the true toll of the coronavirus outbreak.
Giuliana Viglione

A worker digs a grave in a cemetery near Mexico City as the coronavirus outbreak continues. Credit: Edgard Garrido/Reuters
At the beginning of March, Andrew Noymer felt a familiar twinge of doubt. He was watching countries across Europe and North America begin to record their first deaths from COVID-19, and he knew there could be problems with the data. Even in a normal winter, some deaths caused by influenza get misclassified as pneumonia. If that can happen with a well-known disease, there were bound to be deaths from COVID-19 going unreported, thought Noymer, a demographer at the University of California, Irvine. “I just remember thinking, ‘this is going to be really difficult to explain to people’,” he recalls.
And in March and April, when national statistics offices began to release tallies of the number of deaths, it confirmed his suspicions: the pandemic was killing a lot more people than the COVID-19 figures alone would suggest.
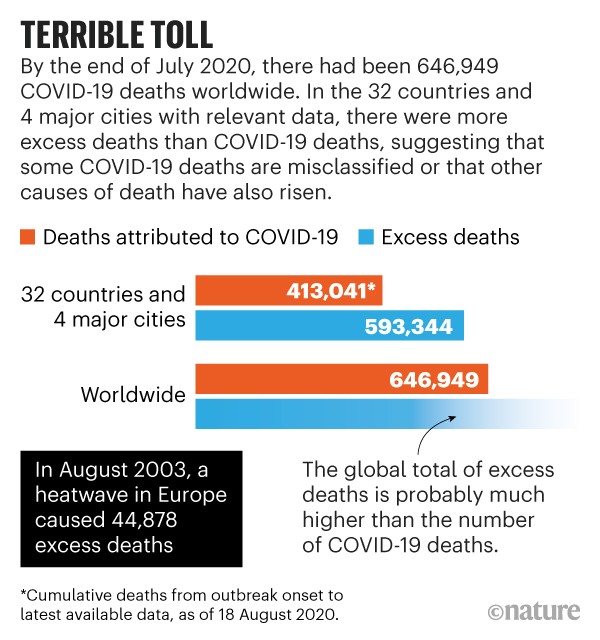
In times of upheaval — wars, natural disasters, outbreaks of disease — researchers need to tally deaths rapidly, and usually turn to a blunt but reliable metric: excess mortality. It’s a comparison of expected deaths with ones that actually happened, and, to many scientists, it’s the most robust way to gauge the impact of the pandemic. It can help epidemiologists to draw comparisons between countries, and, because it can be calculated quickly, it can identify COVID-19 hotspots that would otherwise have gone undetected. According to data from more than 30 countries for which estimates of excess deaths are available (see ‘Terrible toll’), there were nearly 600,000 more deaths than would normally be predicted in these nations for the period between the onset of the pandemic and the end of July (413,041 of those were officially attributed to COVID-19).
Sources: The Economist/The Financial Times/Our World in Data/Eurostat/Human Mortality Database
But this high-level metric has several flaws. It cannot distinguish between those who are dying of the disease and those who succumb to other factors related to the pandemic, such as disruptions to regular health care, which can delay treatments or mean that people do not seek medical care. It relies on accurate, timely reporting of deaths, which can be limited owing to underdeveloped death-registration systems, or might even be intentionally suppressed. And as with so many other aspects of the pandemic, the statistic has become politicized — a way for countries to claim superiority over one another.
Experts worry that simple reports of excess deaths have led to premature or faulty comparisons of countries’ pandemic responses, and have largely ignored the situation in low- and middle-income countries owing to a lack of data.
There are more sophisticated ways to categorize mortality to find out how many people were killed as a direct result of infection with SARS-CoV-2, and how many deaths happened because of other factors associated with the pandemic. Eventually, demographers and public-health researchers will have enough granular information from death certificates to do this. They will then be able to assess which interventions worked best, to inform future pandemic responses.
Several media outlets are already crunching the data and drawing such conclusions. Some statisticians argue that, as the first wave of the pandemic recedes in many places, comparisons can — and should — be made between government policies to see how they might have affected mortality. But many experts say that it’s still too early in the pandemic to do this with rigour. The process can be skewed by the random way that some early outbreaks spread and others fizzle out, making analysis complicated until the pandemic has run its course, says Jennifer Dowd, a demographer and epidemiologist at the University of Oxford, UK. “It’s going to be a very long road.”
Blunt tool
When deaths began creeping up in Europe, Lasse Vestergaard was one of the first to notice. Vestergaard, an epidemiologist at the Statens Serum Institut in Copenhagen, leads the European Mortality Monitoring Project (EuroMOMO), which aggregates weekly all-cause death data from 24 European countries or regions. Between March and April, EuroMOMO’s tracker showed tens of thousands more deaths than expected — about 25% higher than the official COVID-19 deaths figure. Infections were slipping under the radar because of a lack of testing, and because different countries counted deaths in different ways — excluding deaths occurring in care homes, for instance. It was nearly impossible to get a true sense of how countries were faring.

Mourners attend a burial in Manaus, Brazil. The country has so far recorded more than 110,000 deaths from COVID-19.Credit: Michael Dantas/AFP/Getty
So researchers, journalists and politicians turned to calculations of excess deaths. Rather than getting bogged down by cause, the metric compares all deaths in a given week or month with the deaths that statisticians predict would have happened in the absence of the pandemic, usually as an average over the previous five years. More-sophisticated versions model how a population is ageing, or how it is changing as a result of immigration and emigration, although these additions can make it tricky to compare countries. Some analyses of excess deaths, such as a 30 July report released by the UK Office for National Statistics, standardize their mortality rates to control for differences in the age structure of populations between different countries (see go.nature.com/3hxa14m). Because officials can register the occurrence of a death relatively quickly if they are not logging the cause at the same time, these statistics can be compiled much faster than can cause-specific data.
Nature gathered figures from several databases maintained by demographers, as well as from trackers run by The Financial Times and The Economist, two of the most comprehensive data sets on excess deaths. Although the coverage is not universal — it lists 32 countries (largely in Europe) and 4 major world cities — it includes many nations with major outbreaks and comprises about two-thirds of the official COVID-19 death toll up to the end of July.
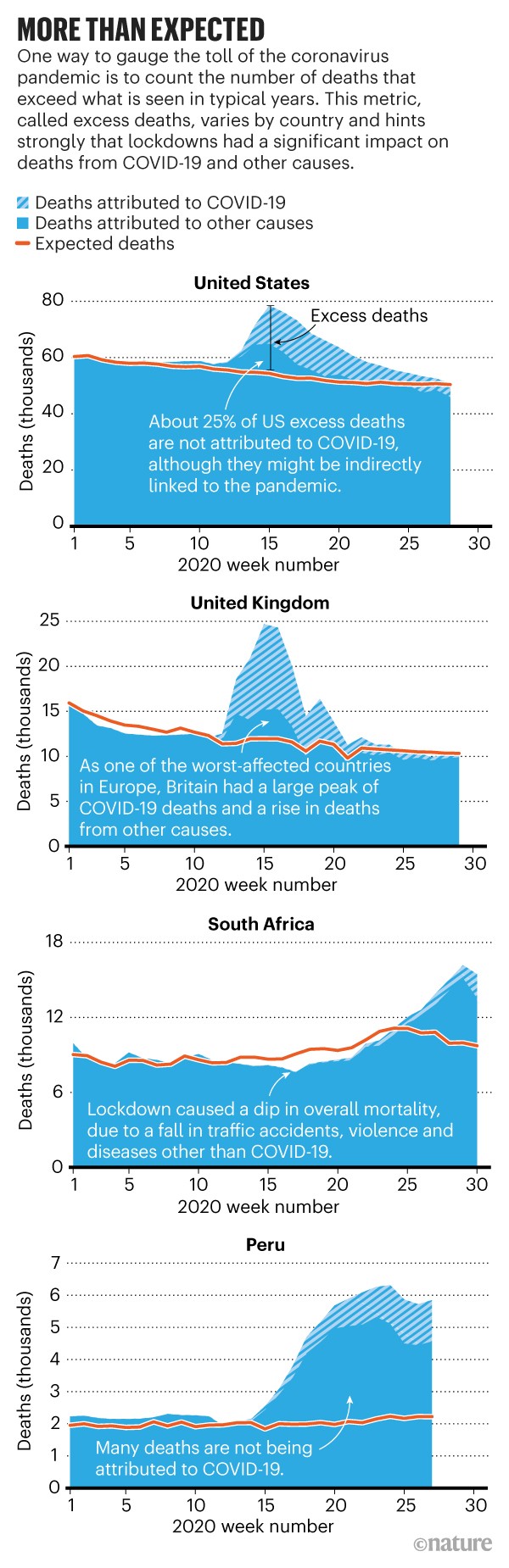
The Nature analysis shows that there are huge variations in excess deaths between countries (see ‘More than expected’). In the United States and Spain — two of the hardest-hit countries so far — about 25% and 35%, respectively, of the excess death toll is not reflected in official COVID-19 death statistics. But in other places, the mismatch is much greater, such as in Peru, where 74% of the excess deaths are not explained by reported COVID-19 deaths. And some countries, such as Bulgaria, have even experienced negative excess deaths during the pandemic so far — meaning that, despite the virus, fewer people have died this year than expected.
Sources: The Economist/The Financial Times/Our World in Data
Digging into data
The blunt tool of excess mortality is the best one to use during the pandemic, say most demographers. But as time goes on, they will be able to use hindsight and more-granular data to improve understanding of the pandemic’s toll. They will eventually be able to parse the deaths into three categories: direct deaths, for which COVID-19 is recorded as the cause; direct-but-uncounted deaths, in which the virus was responsible but wasn’t officially noted; and indirect deaths, which occur because of other changes wrought by the pandemic.
Direct deaths feature on pandemic trackers showing numbers of cases and deaths, which are generally updated daily by local and national health authorities. But even this count isn’t as clear-cut as it might seem, warns Maimuna Majumder, a computational epidemiologist at Harvard Medical School in Boston, Massachusetts.
It can be challenging to differentiate between people who died of COVID-19 and those who were infected but died from unrelated causes. “That’s going to be a very critical piece of all this,” she says. “If you have two concurrent conditions, what does it get classified as?” Parsing those deaths, Majumder says, will require a death-classification system that accounts for the underlying conditions that make COVID-19 more likely to kill. Such a system would mean waiting for cause-of-death data, which take around a year to compile in full.
Researchers are already looking back at the first six months of the pandemic and adding in those deaths that were misclassified at the time. Several major outbreaks, including in Wuhan, China, and in New York City, had their death tolls revised upwards in April to account for deaths that were suspected to have been miscoded.
Then there are the direct-but-uncounted deaths — those that were missed because the individual presented with symptoms not recognized as COVID-19. “We’re still figuring out exactly how the disease manifests,” says Natalie Dean, a biostatistician at the University of Florida in Gainesville. Strokes and pulmonary embolisms are two potentially deadly complications of the virus that might have been overlooked initially, she says.
A small proportion of excess deaths are indirect — a result of the conditions created by the impact of the pandemic, rather than because of the virus itself (see ‘Deaths from other causes’). Some hospitals report that people with cancer and chronic conditions are skipping their regular check-ups, which could put their health in jeopardy. Reports of domestic violence have increased in some places, and researchers who study mental health worry about the toll on front-line workers and those living under lockdown measures — although it’s not yet clear whether there has been a rise in the number of deaths as a result.
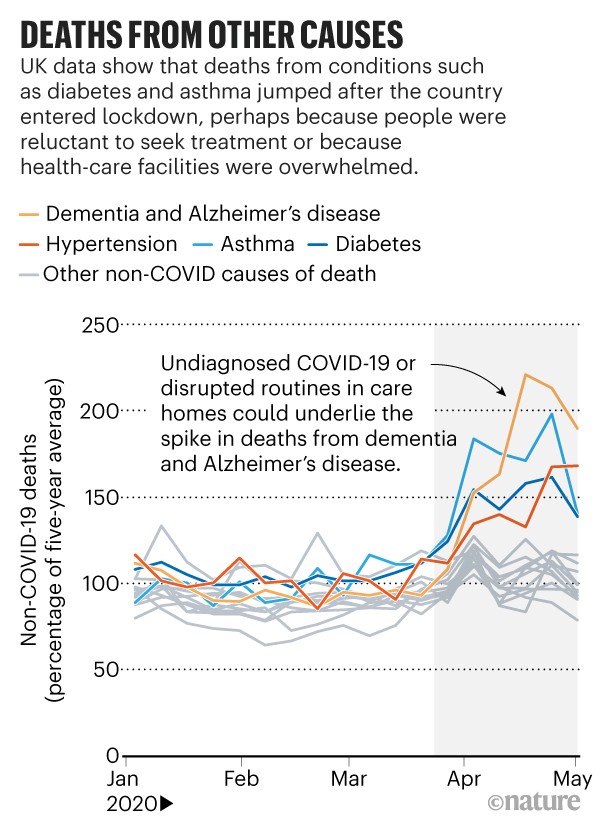
Source: UK Office for National Statistics
Visits to emergency departments in the United States declined by more than 40% in the early days of the pandemic, according to a report from the Centers for Disease Control and Prevention (CDC), suggesting that many people were reluctant to attend (K. P. Hartnett et al. Morb. Mortal. Wkly Rep. 69, 699–704; 2020). And even if they did seek care, hospitals were severely overstretched, Majumder says. “You died from something else, but the reason you died from something else is because the systems that were initially in place to take care of you are no longer strong enough.” Preliminary, incomplete data from the CDC offer a glimpse of these indirect deaths: in April, US recorded deaths from diabetes were 20–45% higher than the 5-year average; deaths from ischaemic heart disease were anywhere from 6% to 29% higher than the norm.
One silver lining is that lockdowns and behaviour changes such as mask wearing and hand washing might have prevented deaths from other causes — particularly other infectious diseases, such as flu. And with large swathes of people staying at home worldwide, deaths from traffic accidents and certain types of interpersonal violence are likely to have diminished. These reductions could be hiding some of the increase in deaths driven by COVID-19.
Some of these effects are already beginning to show up in the data. The global surveillance system FluNet found that this year’s flu season was truncated by more than a month, probably because of strict lockdowns and increased hygiene practices. In South Africa, the death-tracking system put in place during the height of the country’s AIDS epidemic is allowing epidemiologists to distinguish between deaths that are occurring as a result of natural causes, such as disease, and non-natural causes, such as interpersonal violence. A team led by Debbie Bradshaw at the South African Medical Research Council in Cape Town showed that, by the end of March, with strict lockdown measures in place, non-natural deaths had dropped to half their usual number. And when lockdown rules began to lift in late May, these deaths returned to around their expected level.
Demographers will probably never know the pandemic’s final toll with certainty, Noymer says. “You don’t get to scratch off the lottery ticket and find out the actual values underneath the grey plastic coating.” Once the pandemic subsides, disentangling the three types of death — and determining how many would have occurred in the absence of the virus — will be a process that will take months or even years. “We haven’t even settled on how many people died in the 1918 flu,” he says. “And we’ve had 100 years to sort out the numbers.”
Taking stock
Right now, statistics on excess deaths are helping to chart the path of the outbreak in different places. In the future, with full cause-of-death data, researchers will be able to analyse the impacts of lockdowns and other interventions by looking at the levels of direct and indirect deaths from country to country. But it’s risky to do that now, says Noymer, while the pandemic rages on and the final toll is unknown. “We just don’t have much perspective yet, because we’re still in the rising tide,” he says. “It’s like trying to predict rainfall totals in the middle of a hurricane.”
Even after the storm, these analyses will be possible only in high-income countries with robust systems that register births and deaths — known as civil registration and vital statistics (CRVS). In low- and middle-income countries, counting deaths is much less straightforward, says Irina Dincu, a programme specialist in CRVS at the International Development Research Centre in Ottawa. “Across the world, about 50% of the deaths occurring in a given year are registered,” she says. “The other 50% do not exist at all. They are invisible.”
CRVS adviser Gloria Mathenge can think of lots of reasons why these deaths are hidden. In her role at Pacific Community, an international development organization in Nouméa, New Caledonia, Mathenge helps to strengthen data systems in Pacific island countries such as Kiribati and Tonga. Although the situation is improving, about 20% of deaths in the region go unregistered, on average.
Many existing systems are rooted in their countries’ colonial pasts. As a result, Mathenge says, they do not reflect contemporary cultural and social norms — such as the fact that many people in low- and middle-income countries do not die in hospitals. So, in addition to missing COVID-19 deaths, there is no reliable way to establish a baseline from which to calculate an excess.
To estimate the death toll in these countries, demographers will have to rely on less-precise methods such as door-to-door surveys, says Stéphane Helleringer, a demographer at New York University in Abu Dhabi. But these happen infrequently, he says. “By the time we do them, they’re already way outdated.”
For some demographers, it doesn’t necessarily matter whether someone died of the disease itself or because the health-care system was stretched beyond its capacity — all of the deaths can be attributed, in some way, to the pandemic. “At some point you have to say, ‘well that’s COVID-related, somehow, because COVID disrupted the health-care system’,” says Noymer. “To me, the thought experiment is, ‘what does 2020 look like if this thing had never, ever happened?’”
Other researchers are keen to separate deaths caused by the virus from those resulting from circumstance, so that they can build an accurate picture of how lethal the virus itself actually is.
But there’s little time for such analyses right now. The pandemic has drastically increased the strain on death-registration systems as well as the scrutiny they face. Politicians, the media and the public are demanding daily or weekly statistics that would usually take months to compile. That makes some demographers uneasy. “We understand mortality best in retrospect,” Noymer says, because of the time and labour required to compile and analyse death certificates. “Everyone all of a sudden wants to know about it in real time.”
Nature 585, 22-24 (2020)
doi: 10.1038/d41586-020-02497-w
No comments:
Post a Comment